In individuals with suspected WRA who are currently working at the job in question, record.
The tests should be performed using standard recommended protocols and methods supported by European and North American respiratory soci-eties. Changes in airway hyperresponsiveness are best evaluated by comparing tests conducted in the same laboratory. 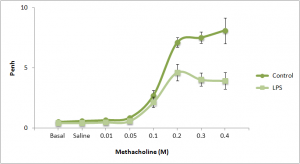
Patient-related factors that impact results include the actual degree of airway responsiveness as well as other factors Generic viagra. The failure to discontinue bronchodilator therapy for an adequate time interval before the test will reduce the measured responsiveness; the effects of current inhaled corticosteroids are less marked (a mean reduction of approximately one doubling dose). A respiratory infection within the 6 weeks prior to testing can increase airway respon-siveness. Repeat tests are best compared when the baseline FEV1 is similar. Exposure within days to weeks before the test to a nonoccupational allergen to which the patient is sensitized can increase airway hyperresponsiveness. Gastroesophageal reflux disease may also impact the results. Such factors must be considered when evaluating changes in responsiveness during periods on and off work. In addition, workers with longstanding OA from a sensitizer to which they are still exposed may have airway remodeling and less acute improvement in airway responsiveness once removed from the work sensitizer. Such patients may have slow improvements in lung function over months or even years away from work.
Although studies have found serial changes in methacholine or histamine responsiveness to be useful as part of the diagnosis of sensitizer-induced OA, few have assessed sensitivity and specificity in comparison to SIC. A study designed mainly to compare serial PEFRs with SIC reported a lower sensitivity and specificity of serial methacholine challenges. Another report noted serial methacholine challenges to be less sensitive and specific compared with SIC. The AHRQ review failed to identify sufficient evidence comparing serial measures of nonspecific airway responsiveness in patients with OA compared with SIC to provide a conclusion on effectiveness.